
History of cardiac or vascular disease was also recorded. Transthoracic two dimensional echocardiography was performed in 12 patients and transesophageal echocardiography in three patients after specific selection criteria (160/90 mm Hg at least twice before the stroke), hypercholesterolaemia (cholesterol concentration >5.2 mmol /l), known diabetes mellitus, and regular cigarette smoking. Four vessel catheter angiography was performed in two patients. Brain MRI consisted of conventional sagittal and transverse T1 and T2 weighted images with 5 mm thick slices, and for 15 patients flow sequence (magnetic resonance angiography (MRA)) centred on the posterior fossa, including the vertebral, basilar, and the posterior cerebral arteries. 6Brain MRI was performed in all patients with presumed involvement of the posterior circulation, following a standard protocol using a Siemens Magnetom 63 SP (Siemens AG Erlanger, Germany) 1.5 T. 6 All the patients had systematic investigations (brain CT, Doppler ultrasonography with B mode echotomography of the carotid and vertebral arteries, ECG, three lead ECG monitoring for at least 24 hours after admission, standard blood tests). We studied 18 consecutive patients with >1 cerebellar infarct, who were included consecutively in the Lausanne Stroke Registry. The aim of our work was to study the clinical, topographical, aetiological, and pathophysiological patterns of multiple cerebellar infarcts. 3-5 However, the association of several cerebellar infarcts in individual patients has not been specifically studied. 2 New types of cerebellar infarcts have also been emphasised (watershed infarcts, very small infarcts). In the New England Medical Center posterior circulation registry (NEMC), over 40% of patients with cerebellar infarction also had infarcts in other territories. 1 Since the advent of CT and more recently MRI, very precise clinical and radiological correlation could be established in the infarcts involving the territory of the main cerebellar arteries, also allowing the recognition of benign and asymptomatic forms. Historically, they had the reputation of a bad prognosis because the first studies were necropsy series. The patterns of multiple cerebellar infarcts have been poorly studied. It is possible that some very small territorial infarcts may be due to a microembolic process, but this hypothesis needs pathological confirmation. It is suggested that these very small territorial infarcts may be endzone infarcts, due to the involvement of small distal arterial branches. Unlike previous series, they could not all be considered junctional infarcts (between two main cerebellar artery territories: 51/91), but also small territorial infarcts (40/91). Our findings emphasised the common occurrence of very small multiple cerebellar infarcts (<2 cm diameter).These very small multiple cerebellar infarcts may occur with (13 patients/18 72%) or without (3/18 22%) territorial cerebellar infarcts. Large artery disease was the main aetiology. Other infarcts in the posterior circulation were present in half of the patients and the clinical presentation largely depended on them. No infarct involved the PICA+AICA combined territory.
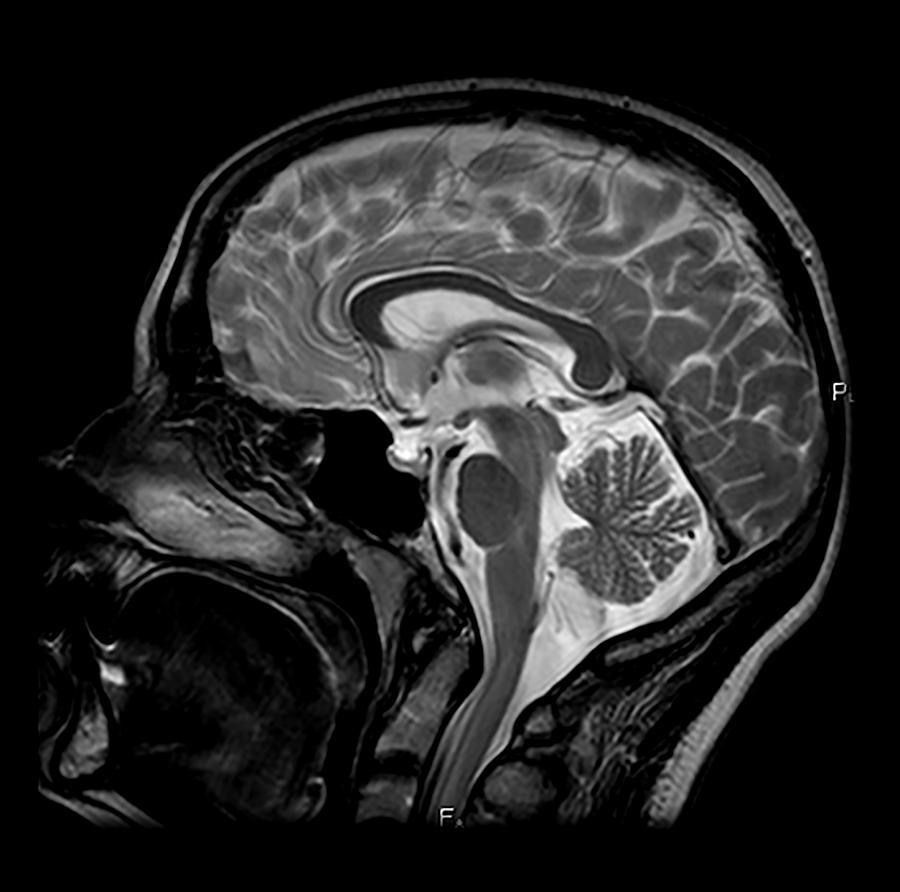
Infarcts in the posterior inferior cerebellar artery (PICA)+superior cerebellar artery (SCA) territory were most common (9/18 50%), followed by PICA+anterior inferior cerebellar artery (AICA)+SCA territory infarcts (6/18 33%). To assess the clinical, topographical, and aetiological features of multiple cerebellar infarcts,18 patients (16.5% of patients with cerebellar infarction) were collected from a prospective acute stroke registry, using a standard investigation protocol including MRI and magnetic resonance angiography.


 0 kommentar(er)
0 kommentar(er)
